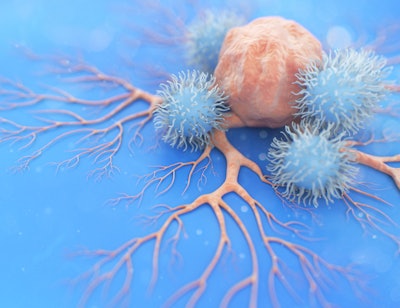
Researchers at Trinity College Dublin, based at St. James’s Hospital in Ireland, have provided new insight into the behavior and metabolic function of a largely unknown immune cell in the lungs. Their findings, published in Proceedings of the National Academy of Sciences, could pave the way for further exploration of these natural killer (NK) cells as a potential treatment for lung diseases, including cancer, COPD and tuberculosis.
Prior to this study, the metabolic function of human tissue-resident NK cells in the lungs was largely unknown. The new findings demonstrate NK cells in the lungs are metabolically different from NK cells that circulate in the blood, said lead author Gráinne Jameson, PhD, in a news release.
“This is impactful because it will enable the investigation of dysfunctional NK cells in respiratory diseases and shows the metabolism of lung-resident NKs is a tractable target for inhalable therapies for many settings of lung disease including cancer and infection,” she said.
These cells, the researchers found, are poised to rapidly respond to increased glucose in the environment, with an enhanced capacity to increase the metabolism of glucose in order to generate materials that the NK cells need to mount an effective immune response.
Other key findings in the research included:
- The lung-resident NK cells exhibit a higher glycolytic capacity compared to non-tissue-resident NK cells. This allows them to generate energy and necessary metabolites more efficiently, enabling a swift immune response.
- The metabolic readiness of lung-resident NK cells indicates they are primed to respond quickly to increased glucose availability during infections, enhancing their ability to mount an effective immune response.
- Understanding the distinct metabolic profile of lung-resident NK cells opens new avenues for investigating dysfunctional NK cells in respiratory diseases, suggesting that metabolism could be a target for immune-supportive therapies in conditions like cancer and chronic infections.
The researchers said one surprising aspect to their findings was the readiness of the lung-resident cells to switch on their glycolytic pathways even before an infection occurs — almost as if they were primed and waiting for a “sugar rush” to activate them.
The next steps in continuing this research will involve exploring additional metabolic pathways involving other nutrients like fatty acids or amino acids, and investigating dysfunctional NK cells and how they become impaired in different respiratory diseases like COPD.