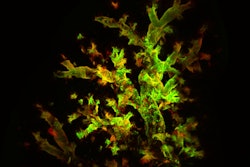
Pulmonologists at the Northwestern Medicine Comprehensive COVID-19 Center (CCC) have made a discovery that could help prevent and treat lung fibrosis. Published in Nature Immunology, the study used gene expression therapy to analyze CT scans from long COVID patients and identify the cause of lung inflammation and injury.
“The underlying cells and molecules that contribute to radiographic abnormalities in long COVID patients are now better established, and equally important, it appears to be the same biological processes responsible for other types of lung injury that result in pulmonary fibrosis,” said senior author Marc Sala, MD. “This common denominator explanation may help not only in developing treatments for long COVID as it continues to evolve in the future, but also contributes to our understanding of pulmonary fibrosis due to other conditions.”
Dr. Sala, who is the co-director of the CCC and a pulmonology and critical care specialist at the Northwestern Medicine Canning Thoracic Institute, said there are currently no FDA- or consensus-approved treatments for long COVID. The breakthrough in knowledge, which will be further validated, could help inform future therapeutic options for the lasting infection and other pulmonary conditions.
Northwestern Medicine researchers collaborated with peers at Brigham and Women’s Hospital, Duke University and The Ohio State University to evaluate 35 long COVID patients at CCC between November 2020 and May 2022. All patients had CT scans showing abnormal lung tissue as well as lingering respiratory symptoms, such as cough and shortness of breath. Of the 35 participants, 26 had been hospitalized with 17 admitted to the ICU.
The specialists labeled the scar tissue, or fibrosis, as respiratory post-acute sequelae of COVID-19 (PASC) with radiographic abnormalities (RPRA). They examined the group of patients to better understand the source of the abnormalities and what was causing them to improve or worsen.
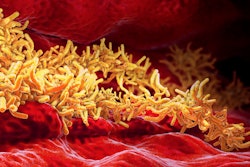
Lung fluid samples showed high levels of pro-inflammatory molecules in patients an average of 5.3 months (but up to 1.5 years) after having COVID. This finding helped explain why immune cells were continuing to migrate into their lungs.
“What surprised us the most was the ongoing flux of pro-inflammatory and pro-fibrotic immune cells from blood into lungs even one year after the COVID infection. Historically, we assume infection-related lung inflammation resolves by this point,” Dr. Sala said in a Northwestern Medicine news release. “The highly overlapping biological processes involving radiographic abnormalities and other non-COVID conditions that lead to fibrosis is an important finding.”
According to the Centers for Disease Control and Prevention (CDC), approximately one-third of COVID-19 survivors develop long COVID and as many as one in 13 U.S. adults experience long COVID symptoms. By recognizing the underlying drivers, researchers can better address, prevent and treat protracted lung inflammation in these patients and people who suffer from fibrosis caused by other pulmonary conditions.
“The more invisible manifestations of long COVID, such as brain fog, shortness of breath, rapid heart rate and fatigue, may well involve similar prolonged inflammation, and this study is an important step forward in supporting this idea,” said Dr. Sala. “The study also supports a broader point that understanding COVID and its ongoing impacts can serve to inform our understanding of other chronic respiratory illnesses that lead to pulmonary fibrosis.”