Scientists have identified a new semi-synthetic compound that could target several drug-resistant strains of tuberculosis (TB). The study was published in Microbiology Spectrum, a journal of the American Society for Microbiology.
Mycobacterium tuberculosis, which is the cause of TB, produces the highest amount of bacterial disease-related deaths worldwide. Current antibiotic treatments are insufficient as they are dated, time-consuming regimens that put patients at risk of developing a drug resistance.
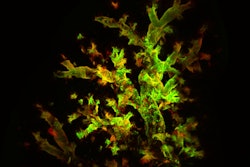
The goal of the study was to discover a new antibiotic that could be effective against numerous defiant strains. The team of researchers zeroed in on sanguinarine, a natural organic compound that is known to have antimicrobial properties. Until now, its toxicity made it unsuitable for use in human drugs, though it has been used in traditional and alternative medicines for animals.
Scientists restructured sanguinarine to develop a less toxic, but effective antibacterial compound called BPD-9. They then tested the therapy in test tubes and mice models, which showed that the drug was able to kill resistant strains of TB. Additionally, they found that BPD-9 was successful in getting rid of intracellular and non-replicating (dormant) M. tuberculosis — two properties that reduce the efficacy of current anti-TB treatments — and was only active against pathogenic bacteria from this genus. This means that the drug could avoid harming the microbiome and beneficial bacteria unlike current antibiotics.
“Our findings show a new chemical entity that has unique properties in combating M. tuberculosis, which may be harnessed further for clinical translation,” said corresponding study author Jim Sun, PhD, in a press release.
“Our finding that the new compound is effective against other members of the Mycobacterium genus may also prove to be valuable in the fight against deadly lung infections caused by non-tuberculous mycobacteria, which are notoriously resistant to most antibiotics. It is also enticing to speculate that BPD-9 could be killing M. tuberculosis in a way that is different than that of existing anti-TB drugs,” said Dr. Sun, who is assistant professor in the department of Microbiology and Immunology at the University of British Columbia.
The study also included bacterial genetics and medicinal chemistry teams from McGill University in Montreal, Quebec, Canada, and the Shanghai Institute of Materia Medica (Chinese Academy of Sciences), and it was supported by grants from the Canadian Institutes of Health Research and the National Sanitarium Association.