A research team from Yale School of Medicine has developed an algorithm to help understand lung disease and propose treatments to slow or reverse the progression of fibrosis. The study, “A Deep Generative Model for Deciphering Cellular Dynamics and in Silico Drug Discovery in Complex Diseases,” was published in Nature Biomedical Engineering.
According to a university press release, the deep generative neural network called UNAGI (unified in-silico cellular dynamics and drug screening framework) can identify patterns in disease-specific data. First, UNAGI analyzes hundreds of thousands of cells to differentiate cell types, isolate genes involved in disease progression and define relevant pathways. Next, the artificial intelligence (AI) model tests various drugs — pulled from a comprehensive list of approved compounds — to propose what treatment works best.
“The model looks for regulation — what characterizes and regulates change —and then, using known drug databases, also suggests treatments,” said co-senior author Naftali Kaminski, MD, of Boehringer Ingelheim Pharmaceuticals, Inc., and professor of medicine (pulmonary) at Yale School of Medicine.
Although researchers used idiopathic pulmonary fibrosis (IPF) data to build UNAGI, the model can be applied to other diseases and states, such as COVID-19 and aging.
Scientists from McGill University in Canada, KU Leuven in Belgium and other institutions collaborated with the Yale team. Previously, Dr. Kaminski and colleagues collaborated to create a technique that can track IPF progression with a single sample, rather than recurring follow-up collection.
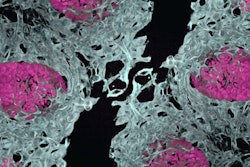
The KU Leuven team collected lungs from IPF patients undergoing transplantation and cut the organs into slices, assigning the pieces to represent different stages of the disease. Then, the Yale team analyzed the samples to rapidly categorize gene expression patterns in more than 230,000 cells and produce a single-cell atlas of IPF.
Dr. Kaminski said the goal was to better understand lung disease trajectory and appropriate courses of treatment. They accomplished this by generating an analytical tool powered by AI and machine learning that could autonomously refine itself over time with new data, which reduces time, cost and manual oversight.
 Naftali Kaminski, MDYale School of Medicine
Naftali Kaminski, MDYale School of Medicine
UNAGI is also able to simultaneously test thousands of drugs with known mechanisms of action and deliver a concentrated list of potential therapeutics.
In this study, UNAGI identified eight drug possibilities, of which one is currently used to treat IPF. From the list, the researchers selected a calcium channel blocker called nifedipine, which is typically used to treat hypertension, but UNAGI predicted it might have anti-fibrotic benefits. When applied to the sample slices of human lung tissue, nifedipine successfully blocked the formation of scar tissue.
While further research is required to examine and validate the model and its proposed treatments, including nifedipine, Dr. Kaminski said, “UNAGI is hitting pathways we did not think about before.”
“We have a convergence of both very sophisticated AI-based analytical methods and the ability to generate data that is high-resolution enough to actually make these observations,” he added.