A team of researchers from Vanderbilt University Medical Center (VUMC) has published a new study that examined gene expression in 35 patients: 26 with pulmonary fibrosis (PF) and nine without. In looking at a unique spatial map that included 1.6 million cells, the data revealed that some lung tissue showed signs of fibrosis prior to the occurrence of significant structural remodeling.
The discovery, detailed in Nature Genetics, could help scientists and doctors better understand the formation of pulmonary fibrosis and be able to detect it earlier, thus improving patient outcomes. It may also indicate future treatment strategies that are based on an individual’s stage of cellular and molecular remodeling.
 Jonathan Kropski, MDVUMC
Jonathan Kropski, MDVUMC
“What we are seeing from this work is the cellular processes that go wrong at the beginning of this disease are not necessarily the things that current treatments would be expected to have any effect on,” Dr. Kropski said in a VUMC news release. “As we get a more nuanced understanding of what is driving these changes, we hope these will lead to clues about what pathways we need to nudge the alveoli back to health.”
Current treatments for pulmonary fibrosis help slow lung function decline but cannot prevent or repair existing damage. Many patients with chronic or severe PF end up requiring lung transplant surgery or die from complications.
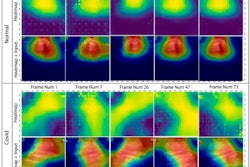
In the study, researchers utilized image-based spatial transcriptomics to distinguish the onset of PF-emergent cell types, determine the cellular and molecular basis of classical PF histopathologic features and detect a range of clear, molecularly defined spatial niches in PF and control lungs.
This technique is critical to studying pulmonary fibrosis, said Dr. Kropski, by allowing scientists to accurately analyze and apprehend the complex cellular process. Next, they compared the lung tissue samples of the control group with those who had PF and had undergone lung transplantation. In total, the scientists profiled 343 genes and identified 12 molecularly defined spatial niches present in both healthy and fibrotic lungs.
“We were intentional in designing this study to make sure we had the ability to look at not just healthy and end-stage disease samples, but also those across a spectrum of pathologic remodeling,” said senior author Nicholas Banovich, PhD.
“[It] gave us the opportunity to determine which cells show changes the earliest — to chart the ‘molecular order of operations’ on how we think disease unfolds, at least on a cellular basis,” said co-investigator Jennifer Sucre, MD, associate professor of pediatrics at VUMC.
The goal of the study, said Dr. Kropski and team, was to bring more clarity to the evolution of pulmonary fibrosis to eventually uncover viable treatment options that better target fibrosis.
“We are excited that these findings give us hope that we may be able to halt or reverse disease by targeting early molecular changes before patients suffer substantial loss of lung function and develop debilitating symptoms from pulmonary fibrosis,” said Dr. Kropski.
The VUMC research group collaborated with investigators from Translational Genomics Research Institute (TGen), based in Arizona, and St. Vincent’s Research Institute in Melbourne, Australia. The team will continue to collect samples and further examine the mechanisms behind pulmonary fibrosis in additional university-led projects.