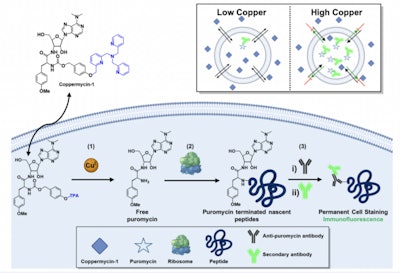
Researchers from Princeton University’s Chang Lab have developed a histochemical, activity-based sensing probe to detect copper in human cells. The innovative tool helps to better understand the role that copper plays in regulating cell growth in patients with lung cancer.
Their study, “A Histochemical Approach to Activity-Based Copper Sensing Reveals Cuproplasia-Dependent Vulnerabilities in Cancer,” was published in Proceedings of the National Academy of Sciences.
According to a Princeton press release, the team suggested the probe could also serve as “a possible treatment modality in which copper chelation shows promising results in certain lung cancers where cells have two related phenomena: a heightened transcription factor responding to oxidative stress and a diminished level of bioavailable copper.”
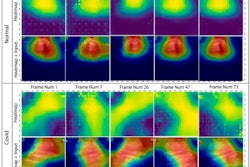
In the study, the lab applied the probe to a panel of human tumor cell lines (obtained from the National Cancer Institute) to isolate cell types that had high levels of copper.
While copper is essential to health, it can cause an imbalance that is involved in cancer cell growth. Researchers have been working to create an instrument that can measure the onset of copper-dependent cell growth (cuproplasia).
“When you think about diseases as complicated as cancer, you really want to understand the fundamentals of what causes an individual cell or collection of cells to live or die. And then you want to bring it back to something that you would use to block or kill that excess growth,” said Christopher Chang, PhD, Princeton’s Edward and Virginia Taylor Professor of Bioorganic Chemistry.
“What we need are more sophisticated biomarkers, and that’s the direction we’ve taken this technology,” said Dr. Chang. “We wanted a method that you could inject in many cell types in parallel, or inject in tissue, and then isolate cancer cells of different types and see which ones had a large or small dependence on cuproplasia.”
The Princeton study validated a direct link between copper and nuclear factor-erythroid 2-related factor (NRF2), which, when activated, promotes gene expression to produce proteins that help prevent cell damage.
 Aidan Pezacki (left) and Christopher Chang, PhDChang Lab
Aidan Pezacki (left) and Christopher Chang, PhDChang Lab
Knowing that patients with certain lung cancers have increased amounts of NRF2, the researchers deduced that the high levels of it and low levels of copper were therefore susceptible to copper chelation. Researchers use chelation therapy to suppress or remove metal nutrients, which lessens the chemical effect and deprives cell growth.
“We took these NCI cell lines and treated them with a copper chelator and then compared cells with either low or high NRF2. What we found was that all the cells with higher NRF2 have higher rates of cell death when we treated with the copper chelator,” said Pezacki. “We suspect that the NRF2 is sequestering copper and then the chelator depletes the cells of copper even further, and this dual deprivation doesn’t keep up with the cell’s need for the nutrient.”
Although these results have not occurred in human tissue yet, the scientists said copper chelation has strong potential as a viable cancer treatment approach, or even other applications.
“This is a proof-of-concept study for profiling metal vulnerabilities in lung cancer. It’s also a platform that we think could be generally applied to not only cancer but the broader process of cell growth,” Dr. Chang said. “All diseases, ultimately, are a question of too much or too little cell growth or cell death. And that’s the elemental balance we’re tracking with this research and the basic science we’re interested in here. It’s part of solving the larger puzzle that goes along with decoding how diet, environment and lifestyle can shape and determine disease states.”