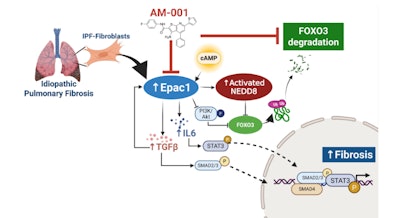
A research team led by the Icahn School of Medicine at Mount Sinai in New York have discovered a previously overlooked protein, Epac1, as a key driver of idiopathic pulmonary fibrosis (IPF), a chronic and progressive lung-scarring condition. The study, “Pharmacological Inhibition of Epac1 Proteins against Pulmonary Fibrosis by Blocking FoxO3a Neddylation,” could pave the way for a new class of treatments targeting Epac1 to help patients before irreversible damage occurs.
The study, which was published in European Respiratory Journal, demonstrated across cell cultures, preclinical models and human lung tissue samples that blocking Epac1 can slow IPF progression.
 Lahouaria Hadri, PhDMount Sinai
Lahouaria Hadri, PhDMount Sinai
Researchers analyzed lung tissue of IPF patients and healthy individuals as well as both cellular and mouse models, confirming that Epac1 is significantly overactive in fibrotic lungs. When they genetically removed Epac1 in mice — or treated the mouse and human lung tissue slices with a small-molecule drug known as AM-001, designed to inhibit the protein — they observed a noticeable reduction in lung scarring and fibrosis.
“This is the first time anyone has shown that Epac1 plays a harmful role in IPF, and that targeting it with a drug can help,” said Dr. Hadri, associate professor of pharmacological sciences and medicine (cardiology) at the Icahn School of Medicine at Mount Sinai. “We were especially encouraged to see these protective effects across all models we tested — from cells to mice to human lung tissue.”
The study also linked Epac1 activity to “neddylation,” another biological process believed to be involved in how proteins are regulated in IPF.
Although the research is preclinical and in early stages, investigators said it opens a new avenue for understanding the molecular underpinnings of the disease. Additional testing and clinical trials are needed before Epac1 inhibitors like AM-001 can be developed into a therapy for IPF patients.
“This research lays the foundation for a completely new treatment strategy. If successful, it could make a real difference for people with IPF, who currently have very few options,” Dr. Hadri said.