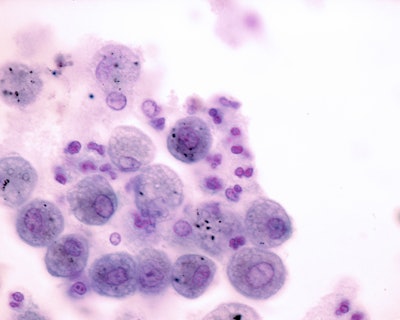
A new study published in Nature Microbiology details how the SARS-CoV-2 infection significantly increases the production of foam cells in human lung tissue. This process is a major contributor to long COVID — the long-term lung damage following infection.
Researchers from the University of Alabama at Birmingham (UAB) and the University of North Carolina at Chapel Hill led the multi-institutional study, “SARS-CoV-2 Infection Induces Pro-Fibrotic and Pro-Thrombotic Foam Cell Formation.”
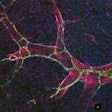
The foam cells, which are made up of lipid-laden macrophages with pro-fibrotic and pro-thrombotic properties, are unique in that they do not occur in other coronaviruses, such as SARS-CoV-1, MERS-CoV or bat-derived strains. The foam cells express genes associated with platelet activation, collagen synthesis and extracellular matrix remodeling, all of which promote persistent pulmonary fibrosis and thrombi formation.
“Our findings underscore the importance of early antiviral intervention to prevent lasting pulmonary injury,” said J. Victor Garcia, PhD, professor and chair in the UAB department of microbiology, in a university press release.
The research team observed that the antiviral molnupiravir (EIDD-2801) when administered early could prevent foam cell formation and reduce fibrosis markers. This suggests the therapy may be effective in mitigating long-term complications from COVID-19, said co-senior author Angela Wahl, PhD, associate professor in the same department as Dr. Garcia.
Additionally, the researchers validated the presence of foam cells in lung tissue even after the virus cleared, indicating the high risk of permanent lung damage for people who sustained mild or moderate COVID-19 infections.
“Foam cells may be the missing link between acute infection and chronic lung complications,” said co-first author Diana Battaglia, PhD, postdoctoral fellow in the Garcia/Wahl laboratory.
 J. Victor Garcia, PhD, Angela Wahl, PhD, and Diana Battaglia, PhDUniversity of Alabama at Birmingham
J. Victor Garcia, PhD, Angela Wahl, PhD, and Diana Battaglia, PhDUniversity of Alabama at Birmingham