A groundbreaking study that evaluates a new method for treating lung cancer has been published in the European Journal of Pharmaceutical Sciences.
Researchers from SINTEF, a large, independent research organization in Norway, have developed a new therapeutic approach that delivers nanomedicines to lung cancer patients via gas bubbles. According to a press release, this unique way of transmitting cytotoxins enables more precise and focused treatments that also are more tolerable.
The research team tested the method on mouse models that were stimulated with cancer. After 30 days of treatment onset, tumors were significantly reduced in size.
“We’re very confident that this approach may offer us a new cure for lung cancer,” said Andreas Åslund, PhD, MSc, a researcher and project manager at SINTEF’s Department of Biotechnology and Nanomedicine. “We envisage that this method of drug delivery can also be used to treat other lung conditions, such as cystic fibrosis, infections and pulmonary emphysema.”
The concept to use the nanomedication technology to treat lung cancer came about by accident, said Dr. Åslund and team. Their original experiment was to use the new system to deliver drugs to the brain and treat brain tumors.
“After a while, we discovered that these gas bubbles ended up in the patients’ lungs,” Dr. Åslund said. “In the first instance, an accumulation of gas bubbles here wasn’t what we wanted, but the discovery meant that we could turn the problem upside down and instead exploit the phenomenon to reach tumors in the lungs.”
Researchers developed a machine that manufactures gas bubbles that encompass the drug-containing nanocapsules. By delivering the medicine at nanoscale and directly to the lung tissue, the treatment is less intrusive, causing fewer side effects for the patient.
“Nanomedicines have the benefit of acting very locally. This makes it possible to treat only the diseased tissue, and also enables us to administer stronger drugs. In so doing, we don’t have to worry about the drugs damaging healthy tissue,” said Dr. Åslund. “It also means that the patient will not suffer as many side effects. It would, in fact, be very dangerous to administer drugs of this efficacy if the doses weren’t so minute.”
Based on the study’s positive results, SINTEF said it has secured a patent for the technology as well as a license agreement with a pharmaceutical company.
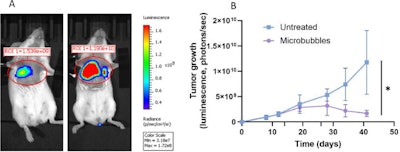 (Above): The mouse on the right received no treatment, while the one on the left was scanned 30 days after microbubble medication treatment began.SINTEF
(Above): The mouse on the right received no treatment, while the one on the left was scanned 30 days after microbubble medication treatment began.SINTEF























