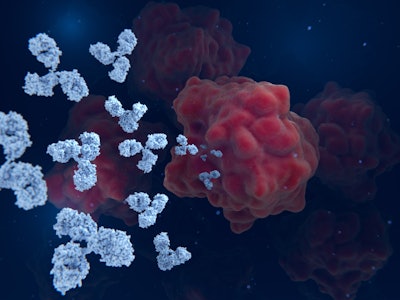
A study, published in Modern Pathology, proposes that HER2 (human epidermal growth factor receptor 2) may help measure and treat lung cancer. The protein is commonly associated as a biomarker for breast cancer, but a new, highly sensitive test shows potential benefits for people with lung cancer.
David Rimm, MD, PhD, and colleagues at Yale Cancer Center developed the novel test, which indicates that more than 60% of lung cancer patients may have enough HER2 to qualify for trastuzumab deruxtecan (T-DXd) — a recently FDA-approved chemotherapy. Previous tests suggested that only 2% of lung cancer patients qualified for the cancer drug that targets HER2, compared to nearly 70% of breast cancer patients. Dr. Rimm said this is because the tests were designed for breast cancer.
 David Rimm, MD, PhDYale School of Medicine
David Rimm, MD, PhDYale School of Medicine
The researchers applied this new, more sensitive test to collected tissue samples from 741 lung cancer patients who had been see at Yale or in Greece during a recent period. Their analysis detected increased levels of HER2 in 63% of lung cancers, which would be enough to qualify an individual for T-DXd therapy.
This is the first advanced test to predict how patients will respond to cancer drugs based on biomarker levels. It is available to order, though it has not yet been approved by the FDA.
In a university news article, Dr. Rimm said he believes the solution will be able to help health care professionals better identify patients who are eligible to receive T-DXd and other cancer drugs. The innovation is an important step on the path of creating and improving personalized medicine, he said.
“Come back to me in three to five years and I think it’ll be a common thing to determine which tag is the highest level, so you can pick that drug first,” said Dr. Rimm.