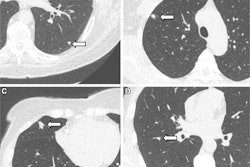
A new observational study, published in The Lancet Respiratory Medicine, identified three distinct blood biomarkers that could help predict severity and prognosis of patients with pulmonary fibrosis (PF). The researchers suggest that this association between PF and certain disease patterns, or endotypes, could improve targeted therapies for the irreversible disease.
The research team, led by Hernan P. Fainberg, PhD, from the NIHR Imperial Biomedical Respiratory Research Centre at Imperial College in London, analyzed blood-derived protein biomarkers of 455 U.K. participants from the PROFILE study. Within this group, 88% had interstitial pulmonary fibrosis (IPF) and 12% had non-specific interstitial pneumonia. The median age was 72.4 years, and the ratio of men to women was 3:1.
Out of the 13 biomarkers that the researchers assessed, three unique clusters stood out. The largest cluster included more than half (248) of participants who displayed high concentrations of basement membrane (BM) collagen neoepitopes. A second cluster of 109 individuals had high concentrations of epithelial injury (EI) biomarkers, and a slightly smaller third cluster of 96 individuals had high concentrations of crosslinked fibrin (X-FIB, or XF).
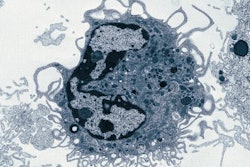
“The biomarkers characterizing each cluster reflect lung parenchymal changes associated with key fibrotic processes — basement membrane repair or dysfunction, epithelial injury and thrombosis,” the authors said. “These clusters could signify distinct endotypes, facilitating patient management and clinical trial stratification regardless of clinical phenotype, age, sex and baseline lung function.”
Within these findings, the team linked the EI cluster followed by the XF cluster with an increased risk of mortality compared to the BM cluster, which demonstrated the best overall survival rates.
“The molecular clusters identified in this study support the existence of distinct endotypes, which might underlie some of the heterogeneity associated with pulmonary fibrosis,” wrote the authors. “The identification of distinct endotypes is an important step in the development of precision medicine approaches. Although there are currently no therapies that specifically target the epithelium or promote basement membrane repair, the availability of anticoagulants offers the potential to improve outcomes for appropriately stratified patients with pulmonary fibrosis.”
Researchers also applied the same machine learning classifier to a replicated dataset from the Australian Idiopathic Pulmonary Fibrosis Registry (AIPFR). Based on extracellular matrix remodeling, epithelial stress and thrombosis, this cohort exhibited the same three clusters as patients from the PROFILE study.