A new lung scanning method has allowed researchers to see how air moves in and out of the lungs in real time in patients with asthma and COPD, as well as those who have had a lung transplant.
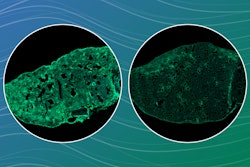
In a study published in Radiology, researchers at Newcastle University, U.K., researchers used a special gas called perflouropropane, which is visible on an MRI scanner. The gas is safe to breathe for patients and once inhaled, scans are taken to see where in the lungs the gas has reached.
Project lead Pete Thelwall, PhD, professor of magnetic resonance physics and director of the Center for In Vivo Imaging at Newcastle University, said in a news release that the new scanning method reveals the parts of the lung that air doesn’t reach properly during breathing.
“Our scans show where there is patchy ventilation in patients with lung disease and show us which parts of the lung improve with treatment,” he said. “For example, when we scan a patient as they use their asthma medication, we can see how much of their lungs — and which parts of their lungs — are better able to move air in and out with each breath.”
By measuring how much of the lung is well ventilated and how much is poorly ventilated, experts can make an assessment of the effects of the patient’s respiratory disease and locate the regions of the lungs that have ventilation defects.
The researchers said the new technique allows clinicians to quantify the degree of improvement in ventilation during treatment, such as an inhaler.
Another study, published in JHLT Open, examined patients who had received a lung transplant for severe lung disease. Study co-author Andrew Fisher, PhD, professor of respiratory treatment medicine at Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University, said the sensitivity of the measurement means medical professionals can spot early changes in lung function, allowing them to identify lung problems earlier and provide better care for patients.
“We hope this new type of scan might allow us to see changes in the transplant lungs earlier and before signs of damage are present in the usual blowing tests,” said Dr. Fisher. “This would allow any treatment to be started earlier and help protect the transplanted lungs from further damage.”