Doctors may be able to detect asthma in the first year of a child’s life by observing a dynamic grouping of symptoms.
In the new study, “Symptom Trajectories in Infancy for the Prediction of Subsequent Wheeze and Asthma in the BILD and PASTURE Cohorts: A Dynamic Network Analysis,” Swiss researchers examined the records of 780 infants born in various European countries. Their analysis showed that a child's risk of developing asthma later in life can be more reliably predicted by observing this grouping of symptoms during the first year of life. The study was conducted by researchers from University of Basel and the University Children’s Hospital in Basel, Switzerland, and published in The Lancet Digital Health.
According to the study’s authors, about one in 10 children has asthma. Genetic predisposition, secondhand tobacco smoke, high levels of air pollution and infections are a few of the risk factors for the condition. Each factor has only a small influence on its own. However, when combined, it makes the odds of having asthma more likely.
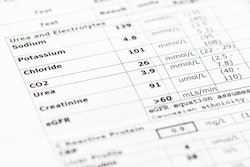
For both cohorts, researchers calculated the network of interactions between a range of known risk factors for every week of each child’s life and then compared them with the appearance of symptoms, such as coughing or wheezing.
“Observing this interaction of risk factors in the context of dynamic development over time is a new way of looking at chronic illnesses,” said researcher Urs Frey, MD, PhD, a chief physician of pediatrics at the University Children’s Hospital in Basel.
It is a case of watching the developing lungs adapting to their environment, he said. In this instance, the adaptation of the lungs differentiated the group of children who developed asthma between the ages of two and six years from those who had not developed it by the time they entered school at the age of six.
“It’s a nice, practical example of the value of digital health data, which were first quantified mathematically using these kinds of dynamic network analyses,” Dr. Frey said.
Although the findings cannot be used for early diagnosis in individual children, Dr. Frey said he believes more data and machine learning could potentially calculate a risk profile for individual children in the future.
Additional research support was provided by the University of Applied Sciences and Arts Northwestern Switzerland and the Inselspital Bern as well as from European partner institutions that were involved in the cohort studies, “Basel-Bern Infant Lung Development (BILD)” and “Protection Against Allergy: Study in Rural Environments (PASTURE).”