ICU patients with comorbid asthma and decreased carbon dioxide (CO2) levels in the blood (hypocapnia) were at a higher risk of in-hospital mortality and intubation, according to researchers from the University of Texas (UT) Long School of Medicine in San Antonio. Their study, “Impact of Arterial Carbon Dioxide Levels on In-Hospital Mortality in ICU-Admitted Patients with Asthma,” was published in the journal, CHEST.
“Asthma exacerbations that lead to ICU admissions are serious and carry a significant risk of morbidity and mortality,” said Sergio Andres Vallejo Avila, MD, an internal medicine resident at UT Health in San Antonio, in an interview with Healio. “Despite advancements in asthma management, we still lack clear, independent prognostic markers that could help predict which patients are at the highest risk for poor outcomes.”
The observational study was designed to explore whether specific markers, such as arterial carbon dioxide (PaCO2) levels, could serve as early indicators of risk in critically ill asthma patients. Researchers examined data from the MIMIC-IV database, looking at patients admitted to ICU departments at Boston’s Beth Israel Deaconess Medical Center between 2008 and 2019 with an asthma diagnosis.
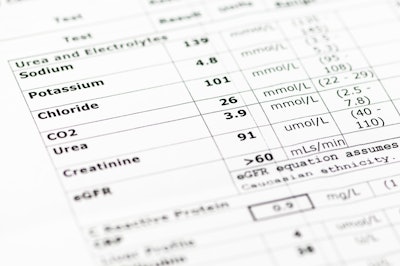
Based on patients’ CO2 levels, researchers further stratified them into two groups. The first group included patients with hypocapnia (CO2 less than 35 mmHg), and the second included patients without hypocapnia (CO2 equal to 35 mmHg).
According to the study’s results, hypocapnia patients had significantly higher in-hospital mortality rates compared with non-hypocapnia patients (27.7% versus 11.5%). Intubation rates were also higher among hypocapnia patients (41% versus 21.8%). There was no significant difference in the length of an ICU stay between the two groups.
 Sergio Andres Vallejo Avila, MD
Sergio Andres Vallejo Avila, MD
Dr. Vallejo Avila said researchers believe the study challenges the traditional understanding of hypocapnia as a compensatory mechanism during respiratory distress and a marker of worse outcomes. It suggests these patients may need more aggressive monitoring and treatment early in their ICU course to avoid fatal outcomes.
“Recognizing this as a risk factor for increased mortality and intubation should encourage closer monitoring and possibly more aggressive interventions, such as earlier ventilatory support,” he said. “Understanding that hypocapnia could indicate more severe disease may lead to earlier interventions that could improve outcomes.”
This study represents an important first step in identifying specific risk factors for ICU-admitted asthma patients, according to Dr. Vallejo Avila. Results support the potential to create a scoring system that could help clinicians stratify patients based on their individual risk profiles. Such a system, he said, could allow for more personalized care, providing patients at higher risk of poor outcomes (due to markers like low PaCO2 or eosinophilia) with more aggressive treatment from the start.