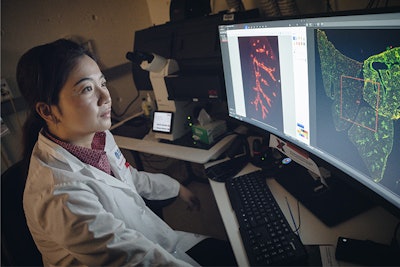
Ke Yuan, PhD, an associate scientific researcher in Boston Children’s division of pulmonary medicine, has long thought that pericytes undergo vascular remodeling and contribute to pulmonary arterial hypertension (PAH). For that reason, the Yuan Lab pursued this hypothesis by identifying a marker to identify pericytes.
“A unique marker to label pericytes would enable us to exclusively study their role in pulmonary diseases,” said Dr. Yuan in a news release.
Pericytes have been historically difficult to study because of their minute size and high variability. They also share markers with several other pulmonary cells, including fibroblasts, myofibroblasts and smooth muscle cells, making them hard to differentiate.
Dr. Yuan’s team previously concluded that pericytes convert into smooth muscle cells aided by hypoxia-inducible factor 2a (HIF2α), of which high levels are known to exacerbate PAH. The team shared the results in a paper, “Pericytes Contribute To Pulmonary Vascular Remodeling via HIF2α Signaling,” in EMBO Reports.
In the 2025 study, “Specialized Pericyte Subtypes in the Pulmonary Capillaries,” published in The EMBO Journal, the researchers identified the marker. They used the gene Higd1b to detect two types of pericytes with two separate reactions to hypoxia. The first pericyte remained dormant, while the second pericyte moved into the arterioles and took on characteristics of smooth muscle cells, thereby contributing to PAH.
This discovery — employing Higd1b to study pericytes — creates opportunities to reimagine therapeutic pathways for PAH and other pulmonary diseases, the researchers said.
“We can use Higd1b as a tracing tool to study how pericytes change their cell fate and location under disease settings such as asthma, COPD and pulmonary fibrosis,” Dr. Yuan said. “This could empower future investigations to delve into the dynamic role of pericytes in disease development and pave the way for disease-modifying therapies.”
Dr. Yuan said the new understanding could also help improve treatments for other conditions, such as heart disease and Alzheimer’s disease, given that pericytes are pervasive throughout the body.























